By Talia Beechick
When Renee Le Verrier saw her first-grade son Pedro paint for the first time 10 years ago, she decided to give it a try, despite recently having been diagnosed with Parkinson’s disease.
“I watched him fill the page, no concern for whether it ‘looked right,’ but with abandon to the process – the colors, the swoosh across the paper,” she said. “I pulled a pear from the fruit bowl and dipped a scraggly brush into his paints. I mixed colors, layered, adjusted the lights. I haven’t stopped painting since.”
Verrier, of the Seattle area, was 43 when she received her diagnosis. She was a book editor who enjoyed writing, sewing, knitting and quilting. It wasn’t until Pedro was in first grade that she felt inspired to pick up a paintbrush. She is one of many for whom art has been a healing force in the midst of a neurodegenerative disease, such as Parkinson’s and Alzheimer’s disease.
Last Thursday, the National Museum of Health + Medicine Chicago hosted an exhibit of artwork created by Lester Potts Jr., who began painting when he was 73 years old, one year after he was diagnosed with Alzheimer’s.
Dr. Daniel Potts, Lester’s son, said his father “was depressed, apathetic, poorly communicative and anxious prior to starting to paint.” The art helped to “give him confidence in himself, improved his affect and depression, made him more communicative, helped his agitation, and seemed to help stabilize his cognitive condition,” the University of Alabama neurologist said.
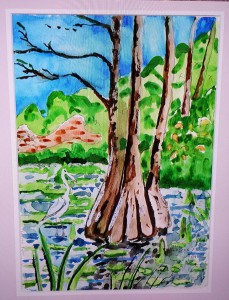
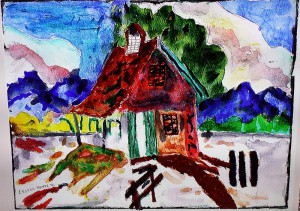
Dr. Potts’ father worked primarily with watercolors and enjoyed painting landscapes, boats, animals and, occasionally, people.
After seeing the success of art in improving his father’s condition, Dr. Potts founded Cognitive Dynamics, a foundation that offers a variety of art-related educational programs for University of Alabama students, middle school students and professional caregivers in residential facilities.
Potts organized an exhibit of his father’s work and debuted it in Beverly Hills before presenting it at the National Museum of Health + Medicine Chicago in June. The exhibit returned to the city for one night last week as part of the museum’s Month of MedTech series, which hosts events each Thursday night through the end of January.
The one-night exhibit also featured a lecture by Elizabeth Barber, a volunteer advocate for the American Academy of Neurology who is developing a company to patent her cancer and Parkinson’s research. She started to research the effects of art and interior design on neurodegenerative patients after her mother was diagnosed with Parkinson’s.
“Therapeutic art stimulates the imagination, it makes people more observant, it enhances our problem-solving skills, it encourages out-of-box thinking, it boosts self-esteem, reduces stress, and enhances cognitive abilities and memory, even for people with serious brain conditions,” Barber said.
She cited studies showing landscapes and horticultural art calms viewers, while familiar images often make viewers feel safe and comforted.
“It offers hope to these patients who, when you look at them, you would think that they can’t do anything, but when they start to paint, they suddenly come alive,” she said.
Registered nurse Cathi Thomas, program director at the American Parkinson Disease Association’s Massachusetts Chapter, agreed. She described several art and movement programs hosted by APDA across the country, including her chapter’s “Painting with Parkinson’s” workshop this year. In addition to improving motor skills and reducing the tremors and stiffness often experienced with Parkinson’s, she noted how art can help patients become more social with family, caretakers and other patients.
Thomas said little scientific research had been done on the topic.
“There are not a lot of studies specific to Parkinson’s, although we do know that there are many studies looking at how art therapy impacts depression and anxiety in the general population,” she said.
Despite the lack of concrete research, however, Thomas said therapeutic art is a growing trend among medical professionals and caregivers alike.
“The trend is increasing, which is a really good thing,” she said. “There’s definitely been an increase in people using art and movement initiatives. People are really thinking outside of the box.”
In 2012, Chicago artist Fabiana Glazer saw the need for therapeutic art and founded GoldMind Arts, a program that hosts workshops and classes at nursing homes, schools and both public and private events. She also has partnered with the University of Chicago’s Memory Center, an outpatient care facility serving individuals with Alzheimer’s or other dementia, to offer weekly art workshops.
“In addition to increased verbalization and decreased confusion and anxiety, people who come to class once a week are more likely to be active outside of class,” Glazer explained. “Also, their relationship with their caregiver dramatically improves. They’re having fun together, there is a reversal of roles, and empathy and communication is improved. Patients are overjoyed.”
Verrier confirmed that art has transformed her experience with Parkinson’s.
“Living with a degenerative disease, no matter how well we manage its symptoms, a reality lingers that is always within grasp: we will get worse,” she said. “Art, on the other hand, is something we can get better at.”